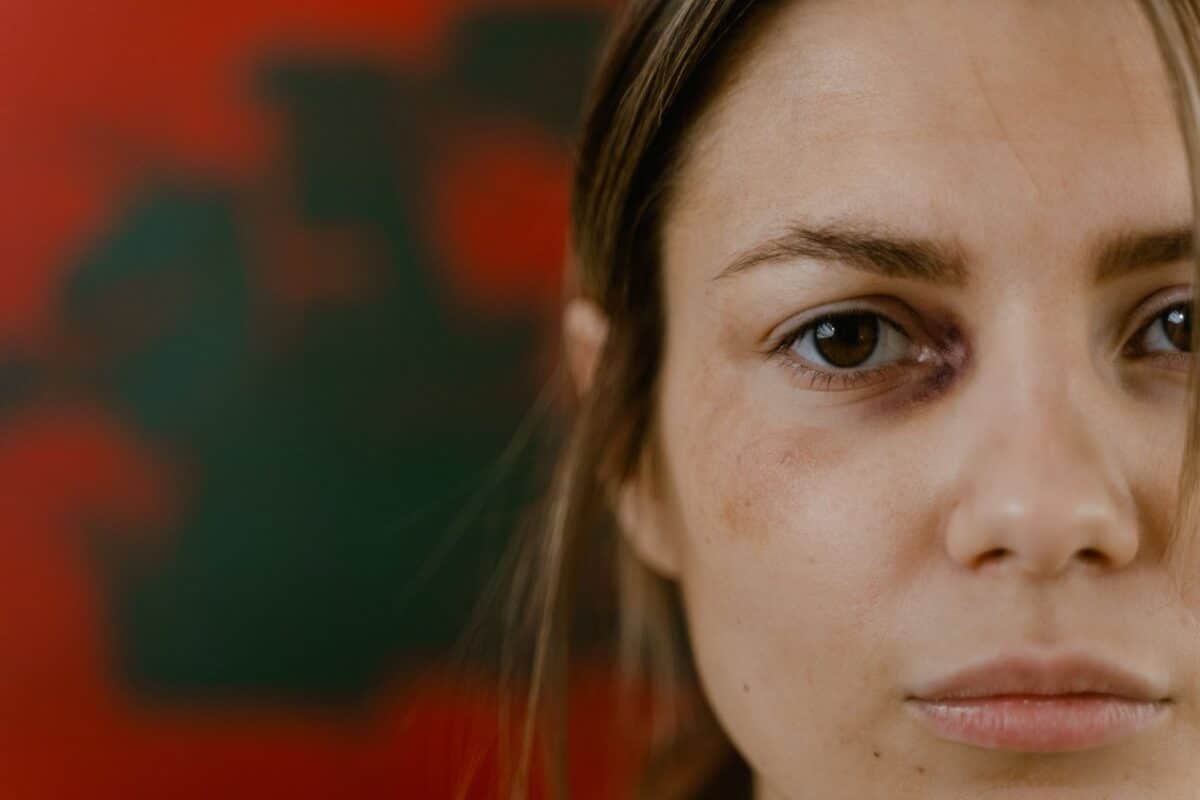
Trauma and depression can walk hand-in-hand. Confronting the aftermath of trauma and the emergence of depressive symptoms is a complex ordeal. The process of overcoming trauma is inherently challenging and can have a prolonged impact on one’s mental well-being, extending far beyond the immediate aftermath of the traumatic incident.
Trauma takes on various forms, ranging from public calamitous events like terrorism to intensely personal experiences such as sexual abuse. Irrespective of the specific nature of the encounter, trauma possesses the capability to deeply disrupt one’s inner equilibrium.
Depression may emerge as a consequence, whether directly or indirectly, of experiencing trauma. However, it is imperative to acknowledge that not all occurrences of depression can be attributed to trauma. The underlying factors contributing to depression are multifaceted, encompassing genetics, environment, and various latent medical conditions.
Navigating the simultaneous coexistence of trauma and depression can be an overwhelming endeavour. Nonetheless, it is vital to recognise that many individuals find solace and fulfilment by employing trauma-focused interventions and receiving support from others.
Can Trauma Precipitate Depressive Symptoms?
In essence, yes. Depression frequently manifests as a prevalent response following a traumatic event.
For instance, a comprehensive research review conducted in 2013 revealed that a substantial 52% of individuals diagnosed with post-traumatic stress disorder (PTSD) also exhibited symptoms of major depressive disorder.
Furthermore, a study conducted in 2015 unveiled a conspicuous link between childhood trauma and the development of depressive symptoms later in life. This study exposed that among 349 individuals grappling with chronic depression, a noteworthy 75.6% disclosed a history of childhood trauma. Notably, those with a background of enduring multiple traumatic events demonstrated an intensified severity in their depressive symptoms.
Depression extends beyond mere feelings of sadness. Instead, it encompasses a spectrum of symptoms, including:
- A pervasive lack of energy
- A diminished capacity for interest and enjoyment in activities previously cherished
- Pronounced fluctuations in body weight
- Prolonged periods of either excessive sleep or insomnia
- Overwhelming guilt
- Impaired ability to concentrate
- Profound feelings of inadequacy
- Repetitive contemplation of death or suicide
It is crucial to acknowledge that not everyone who undergoes a traumatic incident will necessarily grapple with depression or PTSD.
Depression and the Impact on the Nervous System
Traumatic experiences have the potential to exert a profound influence on your brain and nervous system, even in the absence of a formal depression diagnosis.
The emotional response to trauma can significantly affect both the neurological (brain) and physiological (bodily) functions. Trauma can lead to imbalances in brain chemicals and perturbations in the nervous system’s functioning.
When confronted with intense emotional distress or a perilous situation, the body naturally activates the fight-or-flight response as a mechanism to facilitate your escape from the threat.
However, in cases where escape is unattainable, the body resorts to the freeze response, akin to the behaviour of a gazelle “playing dead” when facing an insurmountable predator. According to the polyvagal theory, this freeze state, controlled by a component of the nervous system known as the dorsal vagus nerve, can lead to symptoms akin to depression, such as numbness, disconnection, fatigue, and lethargy. Even after the trauma itself has concluded, prior triggers may induce this state.
What Characterises the Freeze State?
In moments of extreme stress, our bodies shift into survival mode, employing defence mechanisms that mirror the symptoms of depression:
- Out-of-body experiences or dissociation
- A detachment from your surroundings
- Numbness
- Spacing out, with fixed eyes
- A decline in heart rate and blood pressure
- A flat affect, characterised by emotionless facial expressions
- Slowed breathing
- Nausea, vomiting, defecation, or urination
- A lump in the throat, rendering you incapable of speech
- Impaired cognitive function
- Sensations of the body collapsing or curling into a ball
Depression vs. PTSD
Depression and post-traumatic stress disorder (PTSD) are distinct conditions, yet they frequently coexist. The National Center for PTSD has reported that individuals with PTSD are nearly 3 to 5 times more likely to experience depression.
While there is some symptom overlap between depression and PTSD, the two conditions do have differing manifestations. Shared symptoms encompass difficulties with concentration, insomnia, loss of pleasure in previously enjoyed activities, and irritability.
Conversely, PTSD differs from depression in terms of symptoms, which include:
- Reliving the traumatic incident through intrusive memories, nightmares, flashbacks, or heightened reactivity when triggered by reminders
- Avoiding situations reminiscent of the traumatic event
- Developing newfound negative self-perceptions
- Remaining in a hyper-vigilant state, characterised by heightened alertness and a perpetual search for potential threats

Managing Trauma and Depression
Psychotherapy is the recommended approach for addressing both PTSD and depression. Notably, trauma-focused treatments often yield superior outcomes.
Therapies targeting trauma may zero in on intrusive memories, associated thoughts, emotional responses, as well as avoidance and escape behaviours. When seeking help for trauma’s aftermath, it is advisable to consult with a therapist who specialises in or possesses expertise in treating PTSD. They are equipped to deliver tailored therapies that cater to the unique requirements of individuals who have undergone trauma.
Common treatments for PTSD encompass prolonged exposure (PE) and cognitive processing therapy (CPT). For instance, exposure therapy may assist individuals in confronting and managing their fears within a secure therapeutic environment. These techniques are generally not employed to address depression or related disorders.
Psychotherapy for the treatment of depression may concentrate on pinpointing life challenges exacerbating depression and devising strategies for their improvement. It also entails identifying and challenging negative thought patterns contributing to depression, enhancing interpersonal interaction patterns that fuel depression, finding opportunities to engage in enjoyable activities, and integrating a support system into the therapeutic process.
Notably, resolving PTSD can potentially alleviate depressive symptoms without necessitating extensive intervention. However, skills acquired through PTSD treatments like PE and CPT can be effectively applied to manage lingering depressive symptoms after successful PTSD treatment.
Next Steps
The connection between depression and trauma is evident, and while depression and PTSD can share overlapping symptoms, it’s important to understand that they are distinct conditions. Nevertheless, it is essential to grasp that professional help is readily available, and with effective treatment, one need not endure fear, sadness, and extreme stress in isolation.
How White River Manor Can Help
We offer our guests individualised programs and luxury individual care at White River Manor. In collaboration with the client, our team of highly qualified therapists, medical professionals, and dependency specialists work to design a program to restore balance and well-being in our guests’ lives.
If you’d like to talk to us about treatment options and how we can help you recover, please don’t hesitate to reach out to our intake team.







